OTHER COMMONLY ENCOUNTERED MEDICAL
CONDITIONS IN REFUGEE PATIENTS
- Ascaris lumbricoides
Tx
Mebendazole 500 mg once or 100 mg twice daily for 3 days (for patients ≥ 2 years of age)
TOC
Ova & Parasites test 3 months post-treatment
- Enterobius vermicularis (pinworm)
While pinworm infections can be diagnosed using the pinworm paddle test (sticky paddle pressed in the perianal region at night or first thing in the morning), treatment should still be offered prior to obtaining the results of the test in patients with typical symptoms (perianal itching worse at night).
Tx
Mebendazole 100mg once, repeated 2 weeks later (for patients >2 years of age)
Consider treating the entire household if more than one person is infected or in cases of repeated infections.
TOC
Not recommended unless symptoms persist (use the pinworm paddle test).
- Ancylostoma duodenale and Necator americanus (hookworms)
Tx
Mebendazole 500 mg once or 100 mg twice daily for 3 days (for patients ≥ 2 years of age)
TOC
Ova & Parasites test 1 month post-treatment
- Hymenolepis nana
Tx
Praziquantel 25 mg/kg as a single dose, repeated 10 days later
TOC
Ova & Parasites test 1 month post-treatment
- Taenia saginata and solium (intestinal tapeworms*)
Tx
Praziquantel 5 to 10 mg/kg as a single dose
TOC
Ova & Parasites test 1 month post-treatment
* The treatment does not apply to cysticercosis which is a more severe disease caused by the larval stage of T. solium. This topic is outside of the scope of these guidelines.
- Trichuris trichiuria
Tx
Mebendazole 100 mg twice daily for 3 days (for patients ≥ 2 years of age)
TOC
Ova & Parasites test 1 month post-treatment
- Blastocystis hominis
(only treat if the patient is symptomatic)
Tx
Metronidazole 750 mg three times daily for 10 days (children: 50 mg/kg/day divided in 3 doses, max 750 mg per dose)
TOC
Re-test if still symptomatic and if no other cause for the patient's symptoms has been identified.
- Cryptosporidium
Most immunocompetent patients only require supportive treatment (antidiarrheal agents, rehydration) since this infection usually causes self-limited diarrhea. Infections in an immunocompromised individual should be discussed with an Infectious Diseases specialist. For immunocompetent patients (make sure to rule out HIV) with severe acute symptoms or persistent diarrhea (>2 weeks), treatment may be considered, but this requires a special access medication (nitazoxanide) and should also be discussed with an Infectious Diseases specialist.
- Dientamoeba fragilis
(only treat if the patient is symptomatic)
Tx
Metronidazole 750 mg three times daily for 10 days (children: 50 mg/kg/day divided in 3 doses, max 750 mg per dose)
TOC
Re-test if still symptomatic and if no other cause for the patient's symptoms has been identified.
- Entamoeba histolytica* (amebic colitis**)
Consider the risk of spread as well as the risk of invasive disease, all E. histolytica infections should be treated (even if asymptomatic). There are 2 types of medications used for amebic colitis: tissue agents (to eliminate the invading trophozoites) and luminal agents (to eradicate the intraluminal cysts).
Tx for symptomatic patients:
1. Tissue agent:
Metronidazole 750 mg three times daily for 10 days (children 50 mg/kg/day divided in 3 doses, max 750 mg per dose)
2. Luminal Agent (given after the metronidazole course):
Paromomycin 25 to 35 mg/kg/day divided in 3 doses for 7 days
Tx for asymptomatic patients:
Luminal agent only (Paromomycin)
TOC
Protozoal screen 1 month post-treatment
*Entamoeba dispar infections do not require treatment.
** If an amebic abscess is suspected (refugee with fever and right upper quadrant pain), imaging (ultrasound or CT) should be rapidly performed. If an abscess is found, management should be discussed with an Infectious Diseases specialist. Stool microscopy and PCR will usually be negative in patients with amebic abscess.
- Giardia lamblia
Treatment is indicated for symptomatic patients as well as asymptomatic carriers who present a risk of spread (food handlers, child in daycare, household contacts of pregnant women and immunocompromised individuals). Asymptomatic children should also be treated because of the potential impact on their growth.
Tx
1st line*:
Metronidazole 500mg twice daily for 7 days (children: 15 mg/kg/day divided in 3 doses for 7 days, max 250 mg per dose)
2nd line*:
Mebendazole 200 mg orally three times per day for 5 days (for patients > 2 years of age)
TOC
Protozoal screen 1 month post-treatment
* The drugs of choice for giardiasis are tinidazole and nitazoxanide, but these medications are not readily available in Canada. They have to be ordered through the Federal Special Access Programme and should thus be ordered by an Infectious Diseases specialist if the 2 regimens above fail to eradicate a symptomatic infection (giardia can be quite resistant to treatment).
- In Calgary, praziquantel and paromomycin can usually be found at Lukes Drug Mart in Bridgeland.
- Only our preferred first-line treatments are listed above. If these regimens fail to eradicate the GI parasite in question, a referral to an Infectious Diseases specialist is suggested (The Tropical Infectious Diseases Clinics Calgary).
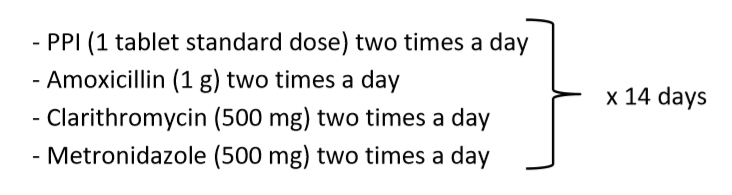
- Proton pump inhibitors: 14 days
- Antibiotics: 28 days
- Bismuth preparations (Peptol Bismol): 14 days
- If
H. pylori
is not identified as the cause of the patient’s dyspepsia or if treating the infection does not resolve the symptoms, refer to the Calgary Zone Primary Care Network
Enhanced Primary Care Pathway for Dyspepsia for a stepwise approach to dyspepsia*.
* The flow diagram on page 4 is especially useful. Since H. pylori is so prevalent in refugee patients, we tend to do step 4 (H. pylori test-and-treat) before step 3 (Baseline investigations) in this population. - Also refer to the American College of Gastroenterology (ACG) and the Canadian Association of Gastroenterology (CAG) 2017 joint guidelines on dyspepsia for more evidence-based recommendations.
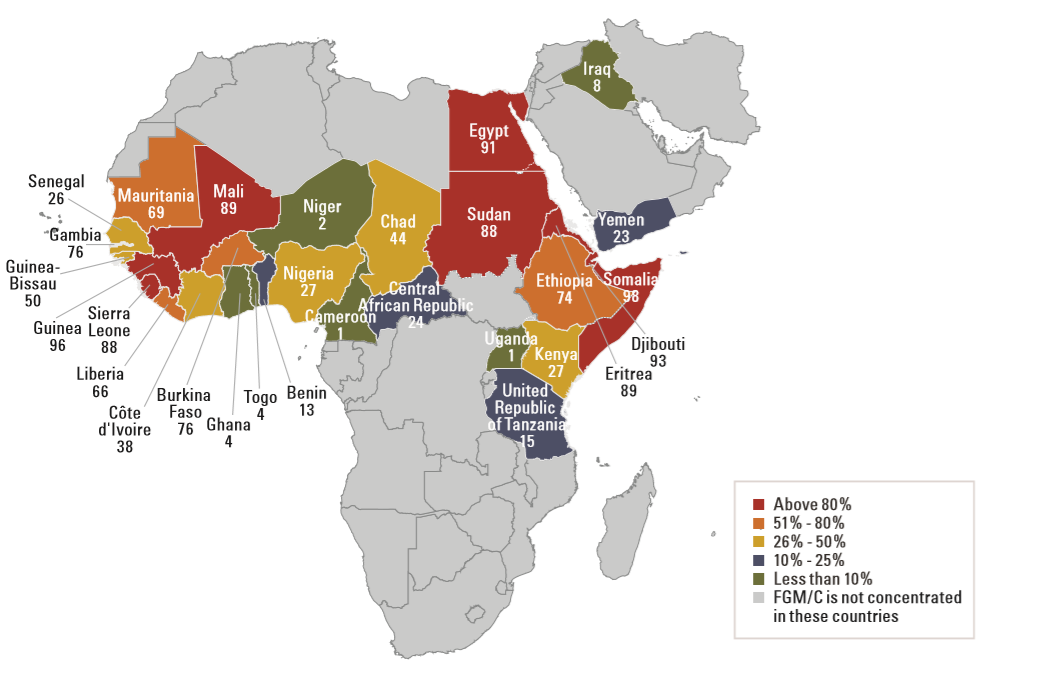
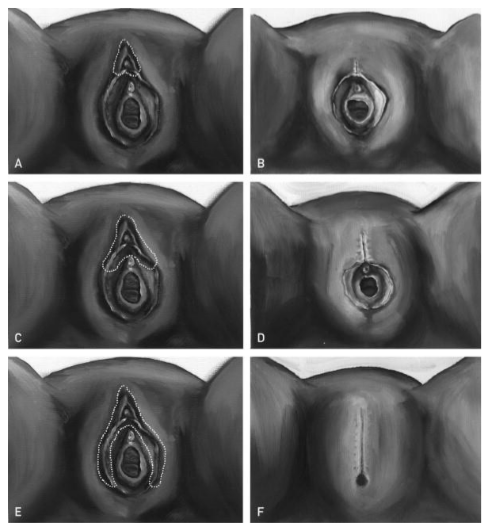
- Prenatal or antenatal patients (in preparation for delivery)
- Patients who will undergo a gynecological procedure (such as a Pap test)
- Any female patient who is from a country where FGM is performed and who has one of the complications/symptoms listed above
- For additional information on hearing screening in refugee children, refer to the Caring for Kids New to Canada website.
Make sure schistosomiasis has already been ruled out as part of the initial screening tests in refugee patients from an endemic country (see Appendix A4). If not, then a schistosoma serology should be ordered. Patients with schistosomiasis and concomitant microscopic hematuria should be treated first before repeating the UA (wait at least 1 month after treatment). If microscopic hematuria is still found on the repeat UA, it is reasonable to re-treat the patient with a second dose of praziquantel since a single dose does not always kill all the adult worms. If microscopic hematuria is still present 1 month after the second praziquantel dose, the patient should then be investigated for another cause of hematuria.
Patients should be asked about any history of macroscopic hematuria* (red or brown urine) and/or blood clots, flank pain, pyuria, dysuria, increased urinary frequency, and urinary retention. Inquire about any past or current smoking history. Ask about any familial or personal history of bleeding disorders and make sure sickle cell has already been ruled out as part of the initial screening process (since both the disease and the trait can cause hematuria). A sexual history should also be performed to assess the risk of STI.
Female patients should also be asked if they had their period during or right before the urine test was performed. Patients should also be asked about any recent history of vigorous exercise or trauma. In these cases, a UA should be repeated with clear instructions: at least a few days before or after the patient’s period, not after any physical exercise, and at least a few weeks after any trauma.
* In patients with macroscopic hematuria, the following steps can still be followed, but a Urology referral should be requested right away.
In patients with microscopic hematuria, order the following tests:
- Repeat UA (to see if the hematuria is transient or persistent*)
- Urine culture & sensitivity and chlamydia/gonorrhea NAAT (if not already done) and treat if positive and repeat UA 6 weeks later
- Serum creatinine levels**
- Urine microalbumin test**
- Renal and bladder ultrasound
** Proteinuria, elevated serum creatinine levels, RBC casts or dysmorphic RBCs on microscopy, hypertension, or "cola" urine suggest glomerular bleeding and a Nephrology referral is recommended in these cases.
Patients with unexplained hematuria who are from a country with a high tuberculosis incidence (see Appendix A5) should be investigated for potential urinary TB. In these patients, at least 3 early-morning (first void) urine samples should be sent for acid-fast stain.Use the CLS Microbiology Requisition to order this test, and write “Acid-fast stain” after “Other - specify:” under the Urine section. A urine mycobacterial culture should also be automatically performed on these samples.
If the patient’s microscopic hematuria is still unexplained after the above investigations, a referral to a Urologist for cystoscopy is then warranted.
- Refer to the Calgary Zone Urology Referral Quick Reference for the referral process of patients with hematuria in Calgary.
- Malaise/chills
- Myalgia/arthralgia
- Tiredness
- Nausea/vomiting
- Diarrhea
- Abdominal pain
- Dry cough
- Sore throat
If malaria is suspected, testing should be ordered as soon as possible. If testing cannot be performed in the community on the same day or if rapid follow-up of the results is not possible (e.g. end of the day or before the weekend), the patient should be sent to the Emergency Department to be tested there. Calgary Laboratory Services have recently changed their testing algorithm. Only one test, a nucleic acid amplification test (NAT), is now performed. This is a very sensitive blood test (97-100%), and malaria smears will only be performed if the NAT is positive. To order this test, you need to order malaria testing under Blood/Sterile Fluids on the CLS Microbiology Form, and complete the CLS Malaria History Form.
- Committee to Advise on Tropical Medicine and Travel (CATMAT) guidelines
- Centers for Disease Control and Prevention (CDC) guidelines
TREATMENT
- Refer to the Canadian Recommendations for the Prevention and Treatment of Malaria by the Committee to Advise on Tropical Medicine and Travel (CATMAT) for more information on the diagnosis and treatment of malaria, including the criteria for severe malaria.
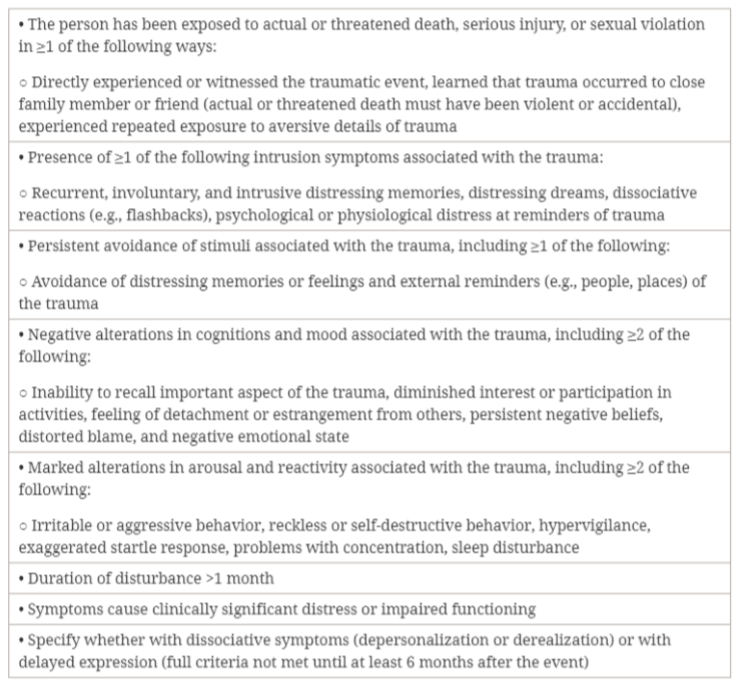
- Had nightmares about the event(s) or thought about the event(s) when you did not want to?
- Tried hard not to think about the event(s) or went out of your way to avoid situations that reminded you of the event(s)?
- Been constantly on guard, watchful, or easily startled?
- Felt numb or detached from people, activities, or your surroundings?
- Felt guilty or unable to stop blaming yourself or others for the event(s) or any problems the event(s) may have caused?
- Address sleep concerns first
If the patient’s sleep is disturbed, we usually start with a trial of prazosin. It works well for PTSD-related nightmares and night-time hyperarousal (can be combined with SSRI or SNRI). We usually start with 1 mg at bedtime and increase the dose progressively. Dose titration differs between men and women: females usually require lower doses, and doses can be titrated up more rapidly in males (see The Psychopharmacology Algorithms by the Harvard Medical School below). Remember that this is an anti-hypertensive agent and thus patients should watch for symptoms of orthostatic hypotension. Prazosin should not be discontinued suddenly because of the risk of rebound hypertension. Trazodone can also be tried if sleep onset is impaired. - Consider a trial of SSRI or SNRI
If symptoms persist after addressing the sleep disturbances or if sleep is not a concern, antidepressants such as SSRIs and SNRIs can be used to reduce PTSD symptoms. We usually start these medications at a low starting dose and titrate up the dose gradually (every 3-4 weeks) until a response is achieved. Doses for PTSD are similar to the ones used for depression. In the literature, the recommended first-line agents are: fluoxetine, paroxetine, sertraline and venlafaxine.
At the Calgary Refugee Health Program, our preferred first-line agent is sertraline because it is usually better tolerated. If sertraline is not effective or not well tolerated, we then recommend trying venlafaxine. We sometimes try venlafaxine before sertraline when the noradrenergic component is needed, rather than the sedating potential of sertraline. We usually avoid paroxetine because of its side effect profile and risk of discontinuation syndrome (which can be a significant issue in refugee patients). Second-line agents are not covered in these guidelines. We suggest not using benzodiazepines in PTSD patients.
- Refer to the Canadian clinical practice guidelines for the management of anxiety, post-traumatic stress and obsessive-compulsive disorders for more extensive guidelines.
- The Psychopharmacology Algorithms by the Harvard Medical School also provide a useful algorithm for the treatment of PTSD, including suggested dosing protocols for prazosin.
TREATMENT
- 10 to 20 kg**: 62.5 mg daily
- 20 to 40 kg: 125 mg daily
- >40 kg: 250 mg daily
- Exclusively breastfed children and children who cannot swallow pills
Ddrops (preferred) or D-Vi-Sol drops 800 UI once daily
- Children who can swallow pills
Vitamin D3 1000 UI tablet once daily
- Adults
Vitamin D2 50,000 UI tablet once weekly*